Adrenal Mass in a Dog
Fiona, a 9-year-old, spayed miniature schnauzer, presented for vomiting and anorexia of approximately 3 weeks’ duration.
History
Fiona’s appetite and activity had waxed and waned over the previous few weeks, and she was not acting like herself. Fiona was up-to-date on annual physical examinations and all vaccinations.
Physical Examination
The examination was unremarkable except for a mildly distended abdomen. In addition, Fiona was panting and appeared nervous.
Laboratory & Imaging Findings
CBC, serum chemistry panel, and urinalysis were unremarkable with the exception of mild elevation in alkaline phosphatase (ALP). The dog’s indirect systolic blood pressure, measured by Doppler ultrasound, was 200 mm Hg.
Related Article: Adrenal Imaging
Abdominal ultrasonography revealed a 3-cm mass in the left adrenal gland with possible compression or invasion of the vena cava. The right adrenal gland appeared normal.
| Which of the following is the most likely diagnosis and most appropriate treatment?
A. Hyperadrenocorticism is most likely; surgery is the treatment of choice.
B. Hyperadrenocorticism is most likely; medical therapy is recommended because most dogs do not survive surgery.
C. Pheochromocytoma only is most likely; medical therapy is recommended because most dogs do not survive surgery.
D. Pheochromocytoma is most likely, but adrenocortical tumor is possible; surgery is the treatment of choice.
E. Pheochromocytoma is most likely, but functional adrenocortical tumor is possible; medical therapy is recommended regardless because most dogs do not survive surgery. |
Best Answer:D. Pheochromocytoma is most likely, but adrenocortical tumor is possible; surgery is the treatment of choice.
Pheochromocytoma is a malignant tumor of the adrenal medulla.1,2 The tumor causes episodic release of excess catecholamines.1,2 Clinical signs, which may be vague and episodic, can include weakness, collapse, restlessness, anxiety, panting, exercise intolerance, decreased appetite, weight loss, and polyuria/polydipsia.1,2 Physical examination findings may include tachypnea, panting, tachycardia, weakness, pallor, arrhythmia, and collapse.1,2
Clinical signs of pheochromocytoma, which may be vague and episodic, can include weakness, collapse, restlessness, anxiety, panting, exercise intolerance, decreased appetite, weight loss, and polyuria/polydipsia.
Related Article: Anesthesia for Adrenal Gland Disease
Diagnosis
In some cases, pheochromocytoma is an incidental finding during abdominal ultrasonography performed because of nonspecific clinical signs or during investigation of another condition. Hypertension can support a diagnosis of pheochromocytoma, but adrenocortical tumors can also lead to hypertension, preventing this finding from being pathognomonic.2
No changes on routine blood work support a diagnosis of pheochromocytoma. The diagnosis is often presumptive, based on clinical signs, physical examination, blood pressure, and the finding of an adrenal mass on abdominal ultrasono graphy. A recent study showed that evaluation of the urine normetanephrine:creatinine ratio may be useful in diagnosing pheochromocytoma.3 However, this is uncommon in veterinary medicine because of limited availability and the handling requirements for the samples. A urine cortisol:creatinine ratio can be evaluated to rule out hyperadrenocorticism.1,2 Depending on these results, as well as serum ALP and clinical findings, a full workup for adrenocortical tumor should be considered during the workup for pheochromocytoma.
Metastasis
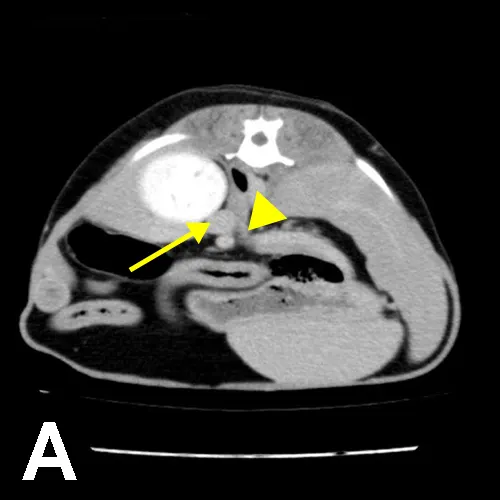
Pheochromocytomas have the potential for vascular invasion and metastasis. The liver and lungs are common sites of metastasis. In all cases, 3-view thoracic radiography should be performed before treatment. Although abdominal ultrasonography is considered an excellent screening tool to evaluate for the presence of adrenal masses and invasion of the vena cava,4 CT is preferred for preoperative planning5 (Figure 1). CT of the thorax and abdomen can determine the extent of disease and evaluate for distant metastasis.
Figure 1. Presurgical CT images of the patient. In the axial view (A), the adrenal mass is visible adjacent to the left kidney (arrow), and extension of tumor into the vena cava is evident (arrowhead). In the coronal view (B), the mass is visible adjacent to the kidney (arrow), but extension into the vena cava is not as obvious.
Medical Treatment
In patients with suspected pheochromocytoma, antihypertensive therapy with phenoxybenzamine should be initiated.6
Phenoxybenzamine, a noncompetitive antagonist of α1- and α2-adrenergic receptors, has been definitively shown to improve perioperative survival in dogs with pheochromocytoma.6 Phenoxybenzamine was administered preoperatively at a median dose of 0.6 mg/kg PO q12h for an average of 20 days6; dogs were 6 times less likely to die in the perioperative period if they were pretreated with phenoxybenzamine.
Surgical Treatment
Surgical removal is the treatment of choice for pheochromocytoma. The reported perioperative mortality is 13% to 50%.1,2,6 The presence of tumor thrombi in the vena cava has been inconsistently shown to increase perioperative mortality.7-10 Patient age, length of time in surgery, development of intraoperative arrhythmias, and tumor size may also play a role in perioperative survival, as they have been found to be negative prognostic indicators.7-10 Generally, an anesthesiologist, surgeon with experience in adrenalectomy, and critical care specialist are the minimum team members required for surgical removal of pheochromocytoma.
Traditionally, this tumor has been approached via midline laparotomy. The mass should be dissected from the peripheral attachments using a combination of blunt dissection, ligation of blood vessels, and electrocautery. Dissection should continue uninterrupted until the mass is free of all attachments except for the phrenicoabdominal vein. If no vascular invasion has occurred, the phrenicoabdominal vein can be ligated and the mass removed.
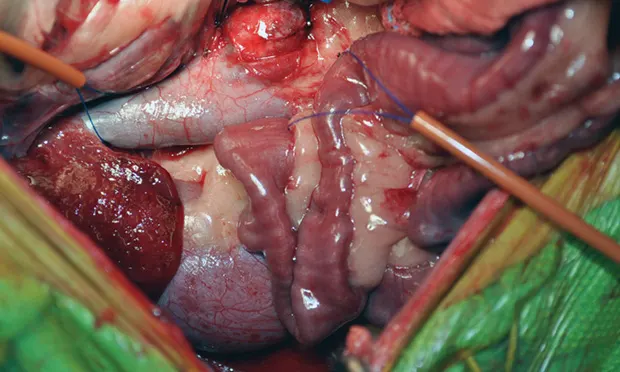
When vascular invasion with tumor thrombus is present, Rummel tourniquets can be placed on the vena cava cranial and caudal to the tumor thrombus and on the contralateral renal vein (Figure 2). The tourniquets should be tightened, cavotomy performed at the level of the tumor invasion through the phrenicoabdominal vein, and the tumor thrombus removed from the vena cava.
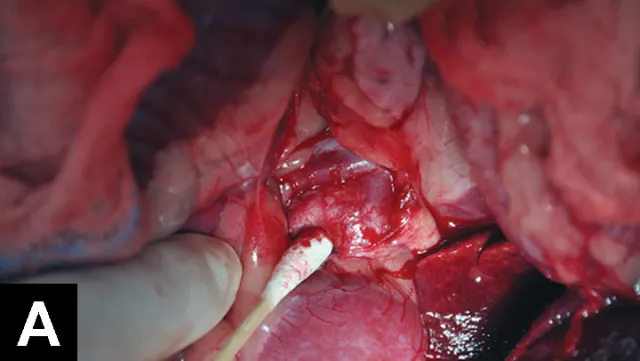
A tangential clamp should then be placed across the venotomy site to allow release of the tourniquets and subsequent partial blood flow through the vena cava. The cavotomy site can be closed and the clamp released. As minimally invasive techniques increase in popularity, laparoscopic removal of select adrenal masses is being used more often.
Figure 2. Intraoperative view of the area of the left adrenal mass before (A) and after (B) dissection. Note placement of Rummel tourniquets (arrows) on the vena cava cranial and caudal to the mass and on the contralateral renal vein in B.
The patient needs to recover in an intensive care unit and be monitored for bleeding, hypertension, hypotension, pancreatitis, and other potential life-threatening complications. Most dogs do well postoperatively, with long-term survival in many cases.
|
Patients with confirmed or suspected pheochromocytoma should be treated with phenoxybenzamine at 0.6 mg/kg PO q12h for an average of 20 days and a minimum of 7 days preoperatively.
A preoperative CT scan of the thorax and abdomen is recommended for local and distant staging and surgical planning.
Surgical removal of pheochromocytoma should involve a multidisciplinary team with experience in adrenalectomy.
|
Outcome
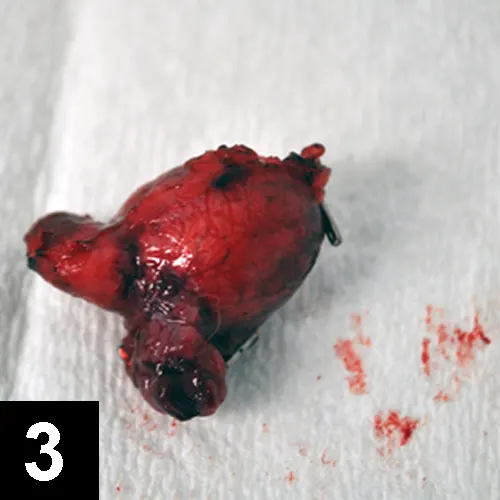
Fiona underwent surgical removal of the affected adrenal gland. A small cavotomy was necessary to remove the area of the tumor invading the vena cava (Figures 2 and 3). She remained hospitalized overnight for monitoring and supportive care and was discharged into the care of the family. At her 6-month postoperative examination, Fiona continued to do well.
Figure 3. The adrenal mass after removal; vascular extensions of the mass are evident.
|
Diagnosis of pheochromocytoma can be challenging because of the vague, nonspecific, episodic signs associated with the tumor.
Abdominal ultrasonography is an excellent screening tool for suspected cases of pheochromocytoma.
Preoperative treatment with phenoxybenzamine has been shown to significantly decrease perioperative mortality and should be initiated before surgical referral.
Although historical reports have indicated that perioperative mortality is high in patients with pheochromocytoma, more recent reports have found that most dogs survive the perioperative period, with prolonged survival in many cases.
|
SARAH BOSTON, DVM, DVSc, DACVS, is associate professor of surgical oncology at University of Florida. She is an ACVS Founding Fellow of Surgical Oncology. Dr. Boston completed her DVM at the University of Saskatchewan and her DVSc and surgery residency at the University of Guelph. She completed a postdoctoral fellowship in Surgical Oncology at Colorado State University.