Acute Respiratory Distress: The Blue Patient
Acute respiratory distress can be broadly divided into 8 categories based on anatomic localization. Several of these can be distinguished by simple observation and physical examination, whereas others require additional diagnostics.
Upper airway obstruction
Lower airway obstruction
Thoracic wall disorders
Pleural space disorders
Pulmonary parenchymal disease
Pulmonary vascular disorders
Abdominal distension
Nonrespiratory disorders (mimics)
Initial Assessment & Diagnosis
Initial assessment of these patients involves observation of the patient’s mentation, posture, and respiratory rate and effort, as well as auscultation of the thorax. Evaluation of the mucous membranes may reveal cyanosis, suggestive of hypoxemia.
Prompt recognition of the underlying reason for respiratory distress is essential to providing appropriate therapy.
Anemic animals may have pale mucous membranes, and cyanosis may not be apparent, even with severe hypoxemia. The pattern of respiration can help localize the problem and guide further diagnostics and treatments.
Categorical causes of hypoxemia include:
Ventilation-perfusion mismatch (pulmonary parenchymal disease)
Diffusion impairment (edema, fibrosis, neoplasia)
Alveolar hypoventilation (airway obstruction, pleural space disorders)
Vascular shunts (right-to-left shunts)
Decreased fraction of inspired oxygen or oxygen concentration (high altitudes).
Upper airway obstructions can lead to inspiratory dypsnea and stridor. Examples of such obstructions include laryngeal paralysis, extrathoracic tracheal collapse, compressive masses, foreign bodies, and brachycephalic syndrome.
Figure 1: Right lateral (A) and ventrodorsal (B) radiographic projections of the thorax of a dog presenting with acute respiratory distress. An alveolar lung pattern is present in the right cranial, middle, and caudal lung lobes, a pattern consistent with aspiration pneumonia. Megaesophagus is present (black arrows), likely leading to chronic regurgitation and secondary aspiration.
Lower airway obstructions result in expiratory dyspnea with auscultable expiratory wheezes. Causes of such obstructions include bronchoconstriction/spasms, inflammation of the bronchial walls (feline asthma, chronic bronchitis), intraluminal exudative/mucoid debris, intrathoracic tracheal collapse and bronchomalacia, or bronchial compression secondary to left atrial enlargement.
Thoracic wall disorders (eg, flail chest, “sucking” chest wounds) can lead to paradoxical respiration with the affected area of the thorax collapsing inward on inspiration and forced outward on expiration.
Pleural space disorders, such as pleural effusion or pneumothorax, can lead to rapid, shallow breathing patterns with inspiratory distress.
Pulmonary parenchymal disorders, such as pneumonia (Figure 1), edema (cardiogenic or noncardiogenic), pulmonary contusions, interstitial lung disease, and neoplastic or fungal infiltration (Figure 2), can lead to both inspiratory and expiratory difficulty. The presence of heart murmurs, gallops, or arrhythmias may suggest underlying heart disease but not necessarily congestive heart failure.
Congestive heart failure can lead to activation of the sympathetic nervous system, which almost invariably results in tachycardia. Primary respiratory disease often induces a vagal response leading to normal sinus rhythms, sinus arrhythmias, or sinus bradycardias.
Pulmonary vascular disorders are most commonly pulmonary thromboembolism and heartworm disease. Clinical signs of pulmonary vascular diseases are variable and include hemoptysis, coughing, dyspnea, and syncope. Other clinical signs may be noted and attributed to the predisposing disease process.1 Split heart sounds may be heard due to concurrent pulmonary hypertension.
Severe abdominal distension can impair diaphragmatic contraction, leading to inspiratory distress that is typically characterized by a slow and exaggerated pattern. Differentials include ascites, gastric dilatation-volvulus, organomegaly, and pregnancy.
Figure 2: Right lateral (A) and ventrodorsal (B) radiographic projections of the thorax of a dog presenting for progressive coughing and acute dyspnea. A diffuse structured interstitial lung pattern is present. Primary differentials would include metastatic neoplasia and fungal disease.

Nonrespiratory diseases that may mimic respiratory distress include acidosis, anemia, pain, and hypotension.
Prioritizing Patient Care
Ensure patent airway
Begin oxygen supplementation (oxygen cage, face mask, intranasal, flow-by)
Obtain vascular access
Perform brief physical examination to identify
♦Mentation changes♦Abnormal mucous membrane color (cyanotic, pale, hyperemic)♦Abnormal respiratory patterns
-Inspiratory distress: Upper airway obstruction, pleural space disorder, abdominal distension, thoracic wall disorders -Expiratory distress: Lower airway obstruction -Mixed: Pulmonary parenchymal or pulmonary vasculature disorder
♦Abdominal distension♦Thoracic wall disorder♦Thoracic findings on auscultation
-Heart rate and rhythm -Abnormal heart sounds -Muffled or adventitious lung sounds
Stabilization
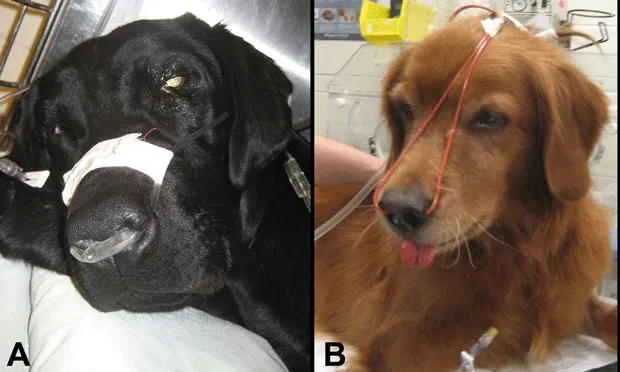
Oxygen supplementation is the cornerstone therapy for the dyspneic patient and is often needed prior to performing a physical examination or diagnostic procedures (Figure 3, see above as article primary image). Several strategies may be used for providing oxygen, with the patient’s temperament dictating the most appropriate method.
The clinician should ensure the airways are patent; otherwise more invasive measures may be indicated (eg, intubation, tracheostomy, mechanical ventilation). In some cases, sedation may be warranted to reduce anxiety associated with respiratory distress. Vascular access should be obtained, if possible, without disrupting oxygen supplementation to allow intravenous administration of medications or fluids if indicated.
Figure 3: Oxygen therapy is the mainstay of treatment for acute respiratory distress and can be provided using a variety of methods. Oxygen cages are the least stressful for the patient but can limit access for further treatments and diagnostic procedures. Intranasal administration of oxygen can be supplied using a nasal prong (A) or red rubber catheters (B) and can provide a FiO2 of 40% to 50% when using 50 to 100 mL/kg per minute of oxygen flow. Face mask and flow-by oxygen can also be used if the patient will tolerate it.
Oxygen supplementation is the cornerstone therapy for the dyspneic patient.
Diagnostics
Initial diagnostics may include:
Blood pressure measurement
Pulse oximetry
Blood sampling to determine packed cell volume, total protein, blood urea nitrogen, creatinine, glucose, and electrolytes
Thoracocentesis if pleural disease is suspected
Fluid analysis of pleural effusion (cytology, cell counts, total protein, and triglyceride/cholesterol concentrations if chylous appearing)
Bacterial cultures of pleural fluid.
Once the patient has been stabilized, additional diagnostics dependent on the clinical situation may include:
Complete blood count, serum biochemical profile, urinalysis
Thoracic or cervical radiography
Echocardiography
Coagulation profile, d-dimer assay
Bronchoscopy and bronchoalveolar lavage
Fine-needle aspiration of the lung
Laryngoscopy
Serial pulse oximetry, arterial blood gas analysis.
Treatment
Specific treatment is targeted to the underlying cause of respiratory distress. Continued oxygen supplementation and preventing stress is vital to avoid further decompensation.
Upper Airway ObstructionSedation with acepromazine (eg, 0.025–0.2 mg/kg IV or IM) or butorphanol (eg, 0.1–0.4 mg/kg IV or IM) may be needed to relieve anxiety and facilitate further evaluation.
If a patent airway cannot be maintained, intubation, tracheostomy, or other invasive measures may be required.
Glucocorticoids (eg, dexamethasone, 0.1–0.25 mg/kg IV) may be needed to reduce laryngeal and pharyngeal inflammation and edema.
Often these patients are hyperthermic and may benefit from active cooling (eg, applying icepacks, cooling fans, cooled IV fluids).
Noncardiogenic pulmonary edema may develop in patients with upper airway obstructions and will require further supportive care.
Lower Airway Obstruction
Bronchodilators (eg, terbutaline, 0.01 mg/kg IM) may be attempted to quickly relieve bronchospasm.
Glucocorticoids (eg, dexamethasone, 0.1–0.25 mg/kg IV or IM) can also be used with acute asthmatic episodes in cats.
Thoracic Wall DisordersPain and concurrent pulmonary contusions from the initiating traumatic event are the likely main contributory factors in respiratory distress.2
Administration of parenteral opioids in combination with local anesthetics (intercostal nerve blocks) may provide more complete analgesia than either alone. Nonsteroidal anti-inflammatories may also be used if no contraindications are observed.
Stabilization of a flail segment (splinting or restraining in lateral recumbency) may lead to improvement in ventilation and facilitate further evaluation and treatment; however, it can also impede the patient’s inspiratory effort.
Intermittent thoracocentesis may be needed initially to relieve a concurrent pneumo/hemothorax until the patient has stabilized or the placement of a chest tube is required.
Specific treatment is targeted to the underlying cause of respiratory distress.
Pulmonary Parenchymal DisordersThoracic radiographs are required for definitive diagnosis and treatment. However, empirical therapy may be necessary initially in extremely unstable patients.
If pneumonia is suspected, therapy includes broad-spectrum antibiotics, such as ampicillin (22 mg/kg IV Q 8 H) and enrofloxacin (10–20 mg/kg IV Q 24 H for dogs and 5 mg/kg IV Q 24 H for cats), pending results of bacterial cultures and nebulization and coupage.
Therapy for cardiogenic pulmonary edema primarily includes a loop diuretic (furosemide, initially 2–6 mg/kg IV or IM) at repeated dosing intervals dependent on the patient’s clinical response. Nitroglycerin ointment (0.25–2 inches transdermally Q 6–8 H) can be attempted to reduce preload in congestive heart failure but absorption is variable.
No specific therapy exists for noncardiogenic pulmonary edema and pulmonary contusions other than supportive care, oxygen supplementation, and mechanical ventilation, if needed. Diuretics are generally contraindicated in this context.3
Pulmonary Vascular DisordersTherapy for pulmonary thromboembolism remains largely supportive but may include a combination of anticoagulants, antiplatelet medications, thrombolytics, bronchodilators, and selective pulmonary arterial vasodilators (eg, sildenafil, 1 mg/kg PO Q 8–12 H; pimobendan, 0.25 mg/kg PO Q 8–12 H) for concurrent pulmonary hypertension.1