Urethral Blockage in a Male Cat: Much More Than Expected
Clifford R. Berry, DVM, DACVR, University of Florida
Gary W. Ellison, DVM, MS, DACVS, University of Florida
Thomas P. Keeshen, DVM, University of Florida

Ivan, a 6-year-old, 6.32-kg castrated Russian blue cat, was referred on emergency for recurrent urethral blockage and stabilization before perineal urethrostomy.
History
A week earlier, because of a urethral obstruction, Ivan had been catheterized by the primary veterinarian and was hospitalized for 2 to 3 days. The cat was discharged on oral marbofloxacin (2 mg/kg PO q24h), meloxicam (0.1 mg/kg PO q24h), and prazosin (0.5 mg/cat PO q12h), but he continued to have difficulty urinating at home; last known urination was 2 days before presentation.
Ask Yourself
How should this patient be treated?
Should surgery be recommended, and if so, when?
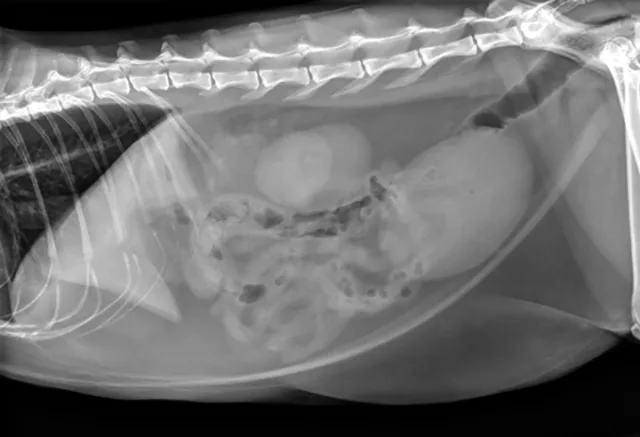
Figure 1. The urinary bladder appears large and there is bilateral renomegaly in this right lateral view; dystrophic mineralization is present in the right kidney.
Physical Examination
At initial examination, Ivan was alert and responsive with heart rate, respiratory rate, and temperature within normal limits. He was estimated to be 5% dehydrated and had a large, firm, nonexpressible bladder. He was sedated with 0.015 mg/kg IV of buprenorphine, 0.2 mg/kg IV of midazolam, and administered a total of 2.5 mL of propofol IV for urinary catheter placement. A 5-French red rubber catheter was placed with slight resistance and maintained in place with butterfly tape and stay sutures. A CBC, serum chemistry panel, and plain abdominal radiographs (Figure 1) were performed.
Diagnostic Results
Initial and subsequent laboratory data showed marked azotemia with elevations in potassium and phosphorus (Table). Urine culture and susceptibility tests were performed; there was no growth on final culture. A urinalysis was not run on initial presentation.
Table. Significant Laboratory Results
Related Article: How to Manage Lower Urinary Tract Signs in Cats
Did You Answer?
Fluid therapy is aimed at correcting dehydration, reversing elevated potassium, and replacing ongoing losses the patient will experience from post-obstructive diuresis.1 Hyperkalemia can be corrected with IV fluids, insulin, and dextrose.2 Calcium gluconate can also prevent some arrhythmias that can form secondary to hyperkalemia.2 This cat was initially stabilized with a 20 mL/kg bolus of lactated Ringer’s solution, 1 mL/kg of calcium gluconate (10%) IV, and 0.2 U/kg of regular insulin IM and maintained on lactated Ringer’s solution and 2.5% dextrose at 3.2 mL/kg/h. Because of severe hematuria and dropping packed cell volume (PCV), Ivan received 2 units of crossmatched packed red blood cells on days 2 and 3 of hospitalization.
Feline idiopathic cystitis is commonly associated with urethral obstruction in male cats.1,3,4 Because this patient had a previous episode of urethral blockage—and because the 2 episodes were close together—perineal urethrostomy was a valid option after correction of azotemia. Plain abdominal films should be taken in feline idiopathic cases to look for cystic or urethral calculi.<sup5sup>
Diagnosis
Initial Treatment & Outcome
Ivan was hospitalized with IV fluids to replace post-obstructive urinary losses and to manage dehydration, azotemia, and hyperkalemia. He also received 0.01 mg/kg of buprenorphine IV q8h. Antimicrobials were not admistered.
The 5-French red rubber urinary catheter was maintained for 3 days; following its removal, the patient produced urine, although he was still pollakiuric, mildly stranguric, and hematuric. An abdominal focused assessment with sonography for trauma (FAST) scan in the emergency room showed a large amount of debris thought to be clots within the urinary bladder. A routine perineal urethrostomy was performed 5 days after presentation.
Ivan initially recovered uneventfully from anesthesia and surgery. The night after his surgery, he was able to urinate without manual expression of his urinary bladder, and he was still hematuric. The next morning, he was started on prazosin (0.5 mg PO q12h). Two days later, he was still able to urinate without aid. Hematuria persisted, and his bladder was moderately full but soft and nonpainful.
Ask Yourself
What findings support a new diagnosis?
What are the treatment options? Is surgical treatment recommended, and, if so, when?
Return
The next morning, 3 days post-surgery, Ivan was seen straining within his cage. At examination, he had a large, firm, slightly painful urinary bladder, and only a few drops of bloody urine were produced on manual expression.
He was mildly tachycardic at 220 bpm. The rest of his vitals were within normal limits, and he had pink mucous membranes. A PCV and blood gas analysis 7 days after unblocking (Table) were within normal limits, but he was still anemic.
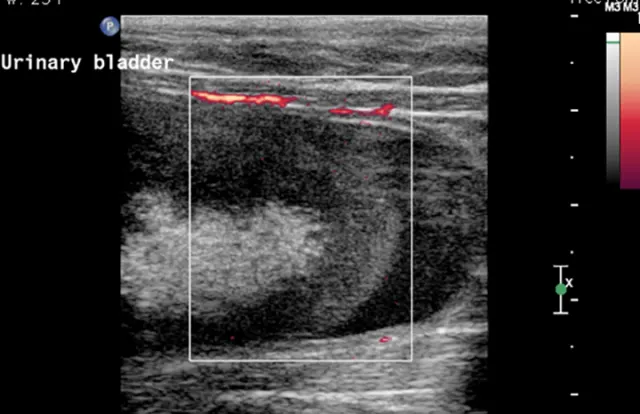
Figure 2. A large echogenic structure is present within the urinary bladder. Power Doppler image shows that there is no blood supply to this material within the urinary bladder.
A 5-French red rubber catheter was easily passed into the urinary bladder, but urine was not recovered. The catheter was initially flushed with 3 mL and subsequently 12 mL of heparinized saline; only 3 mL and 12 mL, respectively, were recovered when aspirated.
A lateral radiograph was repeated and was unchanged from the time of admission.
Additional diagnostic tests included abdominal ultrasound (Figure 2) and computed tomography (CT) scan with IV contrast media (Figure 3).
Figure 3. There is a filling defect taking up the majority of the lumen of the urinary bladder as evidenced by only a thin strip of positive contrast medium present in the periphery of the urinary bladder.

Did You Answer?
Urinary bladder hematoma admixed with sandy calculi was suspected. The structure had no blood flow, which made a neoplastic process less likely. Given the findings of the previous abdominal FAST scan, a urinary bladder hematoma was the top differential.
The choice was made to surgically remove the urinary bladder hematoma via cystotomy. The source of the blood was thought to be renal because of the size and severity of the clot. Ivan was likely continuing to bleed into his urinary tract over the course of his stay because he continued to exhibit hematuria and his PCV continued to drop. This suggested that a moderate-sized bladder after the perineal urethrostomy was actually an organized blood clot, not urine, because there is minimal bleeding from the urinary tract after a perineal urethrostomy. Another option would have been to try to dissolve the clot with tissue plasminogen activator, as is done in humans6; however, given the size of the clot, surgery was decided to be the better option.
New Diagnosis
Treatment
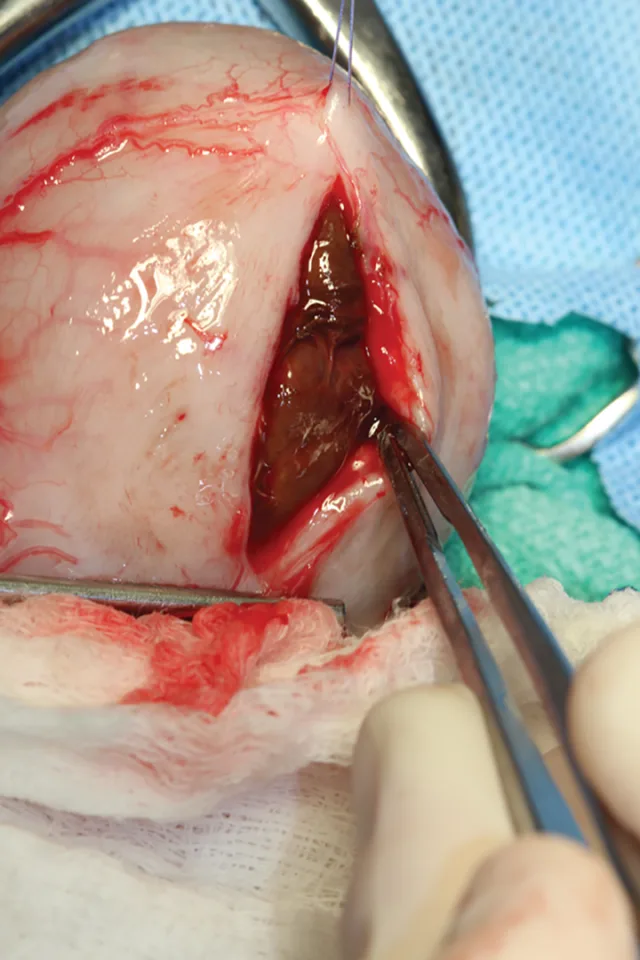
Abdominal laparotomy with cystotomy was performed as the patient was no longer azotemic and his PCV had stabilized around 16% after receiving crossmatched packed red cells (Figure 4). The structure was removed and submitted for histopathology. The diagnosis was an organized hematoma; numerous erythrocytes and moderate numbers of neutrophils and macrophages surrounded by a fibrin layer were seen. Cultures of the bladder hematoma and urine were negative.
Figure 4. A 5 cm × 3 cm semifirm, rubbery structure is visible within the urinary bladder.
Outcome
Ivan was managed postoperatively with a fentanyl CRI at 3 µg/kg/hr and prazosin 0.5 mg q8h. At discharge 2 days later, Ivan had a hematocrit of 10% and poorly regenerative anemia; however, he was bright, alert, and responsive with an excellent appetite and attitude. At 8 weeks after discharge, PCV was 39%, BUN and creatinine were 25 mg/dL and 2.1 mg/dL, respectively, and urine specific gravity was 1.020. In subsequent follow-up conversations with the owner, Ivan appears to have made a full recovery.
Related Article: Stranguria in a Siamese Cat
BUN = blood urea nitrogen, CT = computed tomography, FAST = focused assessment with sonography for trauma, FIC = feline idiopathic cystitis, PCV = packed cell volume