This response is incorrect. See below for the correct answer.
Top 5 Topical Ocular Anti-Inflammatory & Analgesic Agents
Alison Clode, DVM, DACVO, Port City Veterinary Referral Hospital, Portsmouth, New Hampshire
Topical ocular anti-inflammatory agents are essential for many ocular surface and anterior segment intraocular diseases (Table 1). Beyond controlling the potentially vision-threatening consequences of inflammation involving the eye, they also provide analgesia. Drug selection and administration frequency and duration are based on the severity and location of the inflammatory process treated because penetration to the site of action is affected by both disease- and drug-specific factors. Topical administration of medications is rarely indicated for posterior segment (posterior to the lens) diseases because of poor penetration into the posterior segment.
Table 1. Topical Ocular Anti-Inflammatory and Analgesic Agents
*1% tetracaine is available outside of the United States.
1. Corticosteroids
Ocular surface diseases (eg, blepharitis, conjunctivitis, episcleritis, superficial keratitis) may be effectively treated by all topical steroid preparations owing to both their anti-inflammatory and immunosuppressive actions. Of commercially available topical steroid formulations, hydrocortisone has the least potent clinical efficacy, as it is the weakest steroid.1
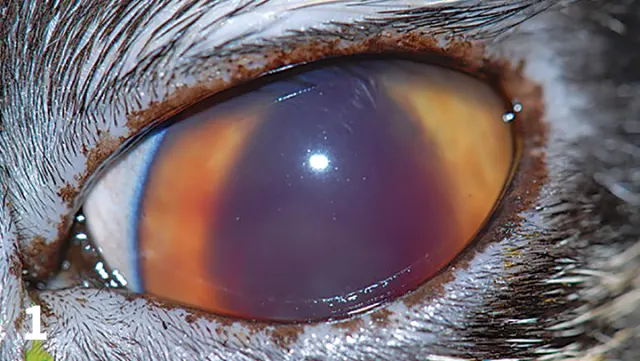
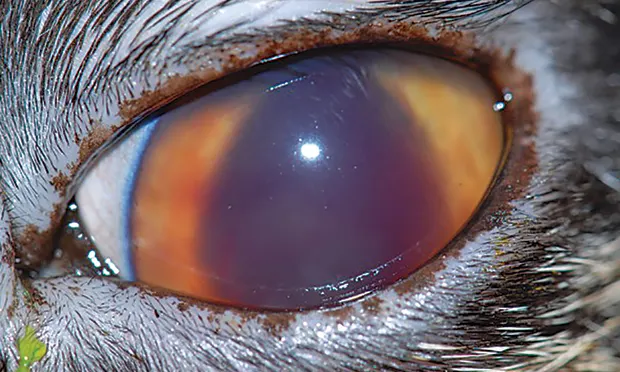
Intraocular inflammation (flare and hyphema obscuring clear visualization of the iridal surface and pupillary margin) in a cat; this condition necessitates treatment with a topical anti-inflammatory.
Deep keratitis and anterior uveitis (Figure 1) are effectively treated only by corticosteroid formulations that penetrate the cornea, which depends on the formulation more than the steroid. Acetate or alcohol preparations demonstrate superior intraocular penetration relative to sodium phosphate preparations, with prednisolone acetate 1% is considered the most effective of the common commercially available preparations.2 Dexamethasone preparations are also appropriate; however, hydrocortisone should not be used for deep keratitis or anterior uveitis because no formulation with either appropriate strength or penetration is available.3
Administration may be as frequent as 4 to 6 times a day, although most disease conditions can be managed with 3 or fewer administrations per day.
Contraindications & Adverse Effects
Topical corticosteroids are contraindicated in the presence of corneal ulceration because they inhibit epithelial healing and potentiate infection. Corticosteroids may also lead to recrudescence of latent feline herpesvirus-1 (FHV-1) infections4; thus, judicious use is important in cats with ocular inflammation. Long-term administration of topical corticosteroids may exacerbate clinical signs of coinciding endocrine conditions (eg, diabetes mellitus, hyperadrenocorticism). Corticosteroids produce lipid deposition within the cornea (lipid keratopathy; generally considered irreversible, but in some patients improvement may be noted after discontinuation) with long-term (weeks to months) therapy, making frequent re-examination and potentially alternative medications necessary.
2. NSAIDs
NSAIDs are potent inhibitors of intraocular prostaglandins, which mediate intraocular inflammation, and thus are beneficial in management of anterior uveitis. Because many forms of blepharitis, episcleritis, and keratitis have an immune-mediated basis, NSAIDs may not be as effective as corticosteroids in the management of these diseases.
The frequency of administration varies with disease severity, with 2 to 3 times per day generally sufficient. Newer topical NSAIDs (eg, bromfenac, nepafenac) have demonstrated clinical efficacy in humans with ocular inflammation5; however, their higher cost often limits use in veterinary medicine.
Contraindications & Adverse Effects
Although safer than corticosteroids in the presence of corneal ulceration, topical NSAIDs should be used with caution, as they may have direct toxic effects on the healing corneal epithelium and may also potentiate infection. Increased intraocular pressure has been reported in dogs6,7 and cats8 following the use of topical NSAIDs.
3. Immunomodulators
Immunomodulators are useful for managing immune-mediated ocular surface inflammatory conditions. Keratoconjunctivitis sicca, chronic superficial keratitis, episcleritis, eosinophilic keratitis, and other immune-mediated keratitides are successfully managed with cyclosporine and tacrolimus9–12 (Figure 2).

Significant corneal vascularization, edema, and fibrosis (without ulceration) in a dog; this condition necessitates treatment with a topical anti-inflammatory, possibly in combination with a topical immunosuppressant.
Intraocular inflammation is not appropriately treated with topical cyclosporine or tacrolimus because of their negligible penetration into the anterior segment of the eye following topical administration.
Sustained-release cyclosporine implants have been developed for surgical placement for treatment of immune-mediated keratitis14 and recurrent uveitis15 in horses.
Contraindications & Adverse Effects
Topical administration of 2% cyclosporine16 has been documented to decrease circulating lymphocytes, but adverse clinical effects have not been reported. Possible effects of cyclosporine on FHV-1 are unknown.
4. Opioids
Topical application of opioids has been investigated for potential use as analgesic therapy for corneal disease. No greater analgesic effect has been demonstrated following topical application of nalbuphine, morphine, or naltrexone relative to either oral opioids or placebo in dogs or cats, nor has nalbuphine been shown to decrease corneal sensitivity in healthy horses.17–21 Thus, topical opioids are not regularly used for analgesic therapy in veterinary ophthalmology.
Contraindications & Adverse Effects
Not only do opioids have limited analgesic effect following topical administration, their possible ocular surface toxicity has not been thoroughly evaluated.

Corneal ulceration with nonadherence of the surrounding corneal epithelial cells. An ulceration such as this necessitates debridement of the epithelium after administration of a topical anesthetic.
5. Local Anesthetics
Topical administration of local anesthetics is critical for diagnostic procedures (eg, tonometry, corneal cytology) and in-hospital treatment (eg, grid keratotomy, conjunctival biopsy) of ocular diseases (Figure 3). Despite their necessity, topical anesthetics should not be administered or dispensed for therapeutic use. Only temporary pain relief is provided, and severe adverse effects (eg, punctate epithelial damage, keratomalacia) can develop with repeated administration. Therefore, after in-hospital use for either diagnostic or surgical procedures, further administration should not be performed.
Contraindications & Adverse Effects
Local anesthetics are toxic to the corneal epithelium, producing lesions ranging lesions that range from punctate epithelial defects to keratomalacia.22