Bacterial Septic Peritonitis
Profile
Definition• Septic peritonitis is an infection of the peritoneal cavity with a pathogenic organism (bacterial, fungal, viral, or protozoal).• Primary septic peritonitis, caused by a spontaneous (hematogenous or lymphatic) source of infection, is rare and usually involves a monomicrobial infection. Such infections can also be caused by device-associated infection (eg, peritoneal catheters).• Secondary septic peritonitis is caused by intraabdominal pathologic abnormalities (eg, intestinal perforation) and is usually polymicrobial (Table).• Feline infectious peritonitis is a syndrome initiated by feline coronavirus; however, it is considered a sterile, nonseptic peritonitis caused by a severe inflammatory and immune-mediated response induced by viremia.
Risk Factors• Recent abdominal surgery• Foreign body ingestion• Trauma (eg, gunshot or other penetrating abdominal trauma, bite wound, vehicular trauma, blunt trauma)• Administration of nonsteroidal or steroidal antiinflammatory agents• Intact male or female (history of recent heat cycle or whelping/queening)• Intraperitoneal chemotherapy• Peritoneal catheter placement
Pathophysiology• Bacteria most commonly associated with septic peritonitis include Escherichia coli, Clostridium species, and Enterococcus species.• The peritoneal cavity becomes infected with a pathogenic organism via translocation, penetrating wound, or leakage from the gastrointestinal tract (most common cause) or an infected organ.• Once pathogens come in contact with inflammatory cells, the production of cytokines and vasoactive substances results in septic peritonitis. This can progress to a systemic inflammatory response that causes vasodilation, extravasation of albumin and plasma water, pain, and hypovolemia. Vomiting, decreased water intake, and fever also contribute to total-body water loss.• The resulting hypovolemic and vasodilatory shock can lead to reduction in splanchnic blood flow, disseminated intravascular coagulation, and multiple organ dysfunction syndrome.• Hypoglycemia induced by sepsis can result in profound weakness, cardiovascular dysfunction, and such neurologic signs as ataxia, seizures, stupor, or coma.SignsHistory• Recent abdominal surgery• Foreign body ingestion• Vomiting, diarrhea, and loss of appetite• Lethargy• Abdominal pain
Physical Examination• Signs of poor perfusion related to shock:- Compensatory: Dogs-tachycardia, red mucous membranes, rapid CRT- Decompensatory: Dogs-tachycardia, pale mucous membranes, prolonged CRT; cats-bradycardia, hypothermia, pale mucous membranes, prolonged CRT• Weak or hyperdynamic pulse quality• Abdominal pain (however, about 50% of cats with septic peritonitis reportedly do not show signs of abdominal pain)• Fever or hypothermia• Abdominal distention (may not bepresent)• Depressed mentation
Pain IndexPain associated with septic peritonitis is usually moderate to high.
Diagnosis
Definitive Diagnosis• Abdominal fluid analysis, including cytologic assessment and aerobic, anaerobic, and fungal cultures, is required. Fluid is most easily collected by using ultrasonographic guidance.• Blind abdominocentesis or diagnostic peritoneal lavage can also be used to collect a sample of abdominal fluid. However, results of a blind abdominocentesis may be negative if < 5 mL/kg of peritoneal fluid is present.• Peritonitis is indicted when abdominal fluid contains a high number of neutrophils. Presence of pathogens typically makes neutrophils appear degenerative or toxic.• Definitive diagnosis of septic peritonitis is made when pathogens are observed. Intracellular or extracellular bacteria may be seen on cytologic examination (Figure 1) or when bacterial or fungal cultures grow pathogens.• If cultures are needed to definitely diagnose septic peritonitis, immediate exploratory surgery may still be warranted; waiting for culture results carries more risk for illness and death than "negative" exploratory surgery.Differential DiagnosisA modified transudate or exudate that is not caused by infection may indicate:• Right-heart failure• Hepatic failure• Hemoabdomen• Leakage of gastric contents (gastric perforation or leakage from previous gastrotomy)• Pancreatitis• Ischemia/necrosis of abdominal organ• Nonseptic uroabdomen or hepatobiliary rupture.
Laboratory Findings & Imaging• Supportive laboratory findings of a septic peritonitis include:- Leukocytosis or leukopenia- Left shift- Hypoglycemia- Abdominal glucose level > 20 mg/dL lower than blood glucose level (dogs)- Peritoneal fluid lactate level > 2.5 mmol/L or a difference < -2 mmol/L between lactate levels in blood and peritoneal fluid (dogs)• Survey abdominal radiographs may show loss of visceral detail, an obstructive gas pattern in the bowel, foreign bodies, or pneumoperitoneum.• Ultrasonographic findings include the presence of abdominal fluid that may appear complex (Figure 2). Other organ abnormalities may be seen depending on the cause of the peritonitis.• When abdominal fluid bilirubin level exceeds the serum bilirubin level, a hepatobiliary tract rupture should be suspected.• When the abdominal fluid creatinine or potassium level exceeds the serum creatinine or potassium level, a urinary tract rupture should be suspected. Contrast urography may confirm a rupture, although urinary tract leaks can seal over and result in negative findings.
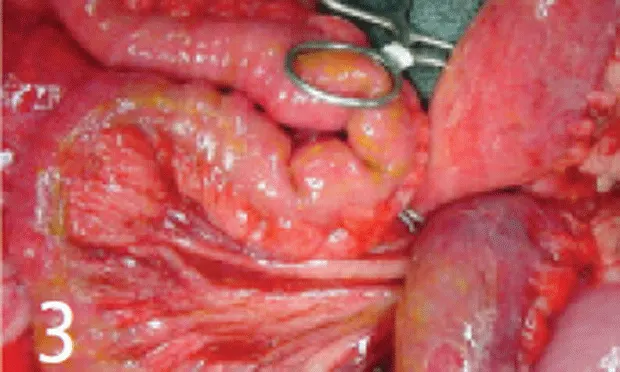
Postmortem FindingsThe abdominal cavity usually contains a large volume of cloudy fluid that is gray, creamy, or red. It may contain flocculent material (Figure 3). The amount of accumulated exudate varies widely; it may spread to the whole peritoneum, or be walled off by the omentum and viscera. The serosal surfaces may adhere to each other, and it is not uncommon to find the omentum adhered to the infected organ. The peritoneal lining and visceral organ surfaces may have petechiae or ecchymotic lesions, and the peritoneal lining may be dull rather than glistening.
Treatment
Inpatient treatment is the only option for bacterial septic peritonitis. Clinical signs of peritonitis warrant rapid fluid resuscitation, analgesia, and rehydration.
Surgery & Lavage• Surgical repair and removal of infected tissue, as well as copious lavage and suction, are required for definitive treatment.• With severe infections, in which ongoing effusion is likely, postoperative abdominal drainage is recommended. Closed abdominal drainage (using active suction drains [eg, Jackson-Pratt drain; cardinal.com] attached to an external reservoir that creates negative pressure) is preferred over open abdominal drainage because it is less labor intensive and more easily managed, allows quantification of accumulated fluid, and permits repeated fluid analysis (Figure 4).• Some surgeons may prefer large-volume lavage (at least 300 mL/kg) and suction before closure of less severe infections, when source of contamination is definitively repaired.• Postoperative lavage cultures provide information on the effectiveness of intraoperative lavage in eliminating infection. In some cases, the exploratory procedure may have to be repeated to reexamine damaged tissue.• If immediate surgery is not possible, a peritoneal lavage catheter can be placed to allow infusion of sterile saline or lactated Ringer's solution to dilute and drain infected contents. Body-temperature sterile saline (10-20 mL/kg) is infused, the abdomen is gently agitated, and the fluid is drained by using passive drainage into a sterile closed-collection system. This process is repeated until the appearance of the fluid clears.
NutritionParenteralPartial parenteral nutrition, infused through a peripheral or central venous catheter, can be provided immediately upon diagnosis and used as the maintenance fluid infusion. Additional balanced isotonic crystalloidsare used to replace ongoing losses.
Enteral• Enteral nutrition using temporary feeding tubes is provided during postsurgical recovery. Immediate enteral feeding may reduce the risk for bacterial translocation and ulceration, and augment mucosal healing in cases of gastrointestinal surgery.• Feeding begins with one third daily caloric needs. Over 48 to 72 hours, intake is increased to full caloric needs.• Because it may take several days for gastric function to return, intermittent gastric tube suction may be needed to reduce vomiting.• Metoclopramide (1-2 mg/kg Q 24 H after a single intravenous dose) and cisapride (0.5-1 mg/kg PO Q 8 H) may promote gastric emptying. In addition, intravenous lidocaine at analgesic doses (see Septic Peritonitis: Analgesic Medications, page 46) may improve gastrointestinal motility in cases of postoperative ileus.• Bypassing the stomach and feeding through nasojejunal or jejunostomy tubes can permit enteral feeding until gastric function is restored.• Experience is needed to properly place gastrostomy or jejeunostomy feeding tubes. Placement of nasogastric, nasojejunal, or esophageal tubes requires less experience, and these tubes do not necessitate surgery if they become prematurely removed.
Length of CareAt least 3 to 5 days of hospitalization is often necessary when treating septic peritonitis. Reexploration may be necessary in some cases, and owners should be told of this possibility at the time of the initial surgery.
Medications
FluidsLoss of proteins and large volumes of plasma water into the abdomen and gastrointestinal tract is common.• Initial fluid resuscitation should include balanced isotonic crystalloids and synthetic colloid (hetastarch) administration. See the Management Tree, page 61, for an approach to treating hypovolemic shock.• After correction of the underlying cause, restoration of normal fluid balance takes 2 to 5 days. Because albumin becomes an ineffective colloid in patients with systemic inflammatory response syndrome, use of hetastarch, which contains large heavy-weight colloid molecules, permits maintenance of intravascular colloid osmotic pressure and reduces loss of intravascular fluid into the peritoneal cavity.• The volume of plasma transfusions required to restore plasma albumin levels in the patient with septic peritonitis makes this therapy costly, increases patient risk for fluid overload, and drains transfusion product reserves.• Use of human albumin concentrate to replace albumin is controversial in septic veterinary patients due to the risk for acute and delayed hypersensitivity reactions in dogs. Although there is a theo-retical benefit to maintaining albumin homeostasis, no controlled studies have evaluated the benefit of maintaining plasma albumin levels in septic peritonitis cases.• Frozen or fresh frozen plasma may be necessary when coagulation factor deficiencies result in bleeding tendencies.
Analgesia• Pure agonist opioids can be used intravenously. Intravenous benzodiazepines, low-dose ketamine, and lidocaine can augment opioid analgesia. Continuous intravenous infusion after a bolus injection provides continuous analgesia that can be modified according to patient needs.• The greatest relief may be obtained with epidural analgesia using morphine with or without local anesthetics. Longer-term analgesia can be administered by using an epidural catheter.• Nonsteroidal antiinflammatory analgesics are not administered until gastrointestinal integrity and renal function are determined to be normal and hypotension is not considered a concern. Alpha-2 agonists are avoided until cardiovascular stability is ensured.
Antibiotics• Once culture samples have been obtained, broad-spectrum IV antibiotics are provided for common enteric pathogens such as gram-negative and anaerobic bacteria. Examples include ampicillin-sulbactam with metronidazole, or first-generation cephalosporins with aminoglycoside and metronidazole. Second- and third-generation cephalosporins and fluoroquinolones are reserved for documented resistant infections.• Aminoglycosides are used with close monitoring of renal function. Amikacin (15 mg/kg IV Q 24 H) may be preferred over gentamycin in renal-compromised cases. Daily examination of the urine for casts, glucose, and protein can reveal renal tubular injury. In addition, daily comparison of the urine gamma-glutamyl transferase:creatinine ratio with baseline values may uncover early renal toxicity in the dog. Maintaining hydration and renal perfusion will reduce risk for toxicity.
Follow-Up
MonitoringPostoperative monitoring should include evaluation of Kirby's Rule of 20 (page 42). These are clinical variables that must be addressed in the critical patient once or twice daily to maximize recovery and minimize complications by anticipating alterations in organ function.
ComplicationsComplications can include adhesion formation, dehiscence, and persistent or secondary infection.
Prognosis & Home CareA favorable prognosis is expected when the patient is eating and drinking without vomiting, afebrile, and comfortable 2 to 5 days after surgery. At-home treatment generally consists of analgesia and a bland diet for the week after discharge, and antibiotics until final culture results are documented. Patients are occasionally discharged with feeding tubes until they are voluntarily eating adequate amounts of food.
Future Follow-UpFurther follow-up is usually needed only for removal of feeding tubes and sutures.
In General
Septic peritonitis requires major abdominal surgery and intensive care ($$$). Survival rates are reported to be about 70% for bacterial peritonitis in dogs and cats regardless of the method of drainage, and 54% for cases that are lavaged and closed without drainage. Prognosis is good when early surgical intervention is provided and septic shock avoided.
Causes of Secondary Septic Peritonitis
Gastrointestinal tract
Perforating foreign body
Mass rupture
Ulcer perforation
Ischemia
Surgical wound dehiscence or leakage
Translocation through inflamed intestinal wall
Pancreatic abscess
Genitourinary tract
Urinary tract rupture with existing infection
Uterine rupture
Pyometra
Prostatic abscess
Renal abscess
Hepatobiliary leakage with existing infection
Necrotizing cholecystitis
Biliary mucocele
Liver lobe torsion
Hepatic abscess
Other
Penetrating abdominal wall trauma
Evisceration
Surgical contamination
Splenic or lymphatic abscess
Peritoneal dialysis
BACTERIAL SEPTIC PERITONITIS • Elke Rudloff
Suggested ReadingAbdominocentesis and diagnostic peritoneal lavage. Rudloff E. In Ettinger S, Feldman E (eds): Textbook of Veterinary Internal Medicine, 4th ed—Philadelphia: WB Saunders, 2005, pp 269-270.Comparison of peritoneal fluid and peripheral blood pH, bicarbonate, glucose, and lactate concentration as a diagnostic tool for septic peritonitis in dogs and cats. Bonczynski J, Ludwig L, Barton L, et al. Vet Surg 32:161-166, 2003.Crystalloid and colloid fluid therapy. Kirby R, Rudloff E. In Ettinger S, Feldman E (eds): Textbook of Veterinary Internal Medicine, 4th ed—Philadelphia: WB Saunders, 2005, pp 412-423.Diagnosis and management of peritonitis. Swann H, Hughes D. Vet Clin North Am Small Anim Pract 30:603-616, 2000.Lactate as a diagnostic test for septic peritoneal effusions in dogs and cats. Levin G, Bonczynski J, Ludwig L, et al. JAAHA 40:354-371, 2004.Open peritoneal drainage versus primary closure for the treatment of septic peritonitis in dogs and cats: 42 cases (1993-1999). Staatz A, Monnet E, Seim H. Vet Surg 31:174-180, 2002.Peritoneum and peritoneal cavity. Kirby B. In Slatter D (ed): Textbook of Veterinary Surgery, 3rd ed—Philadelphia: WB Saunders, 2003, pp 414-445.Septic shock. Kirby R. In Bonagura J (ed): Kirk’s Current Veterinary Therapy XII—Philadelphia: WB Saunders, 1995, p 139.Surgery of the abdominal cavity. In Fossum T, Hedlund CS, Johnson AL, et al (eds): Small Animal Surgery, 3rd ed—St. Louis: Mosby Elsevier, 2007, pp 317-338.Techniques for the septic abdomen. Bentley A, Holt D. In Silverstein D, Hopper K (eds): Textbook of Small Animal Critical Care—Philadelphia: WB Saunders, 2008, pp 72-76.Underlying cause, pathophysiologic abnormalities, and response to treatment in cats with septic peritonitis: 51 cases (1990-2001). JAVMA 225:897-902, 2004.Use of closed-suction drains to treat generalized peritonitis in dogs and cats: 40 cases (1997-1999). Mueller M, Ludwig L, Barton L. JAVMA 219:789-794, 2001.