Differentiating Nuclear Sclerosis From Cataracts
Alison Clode, DVM, DACVO, Port City Veterinary Referral Hospital, Portsmouth, New Hampshire

Cataract development is a significant cause of vision impairment and blindness in dogs and cats, resulting from alterations in the nature of crystalline lens proteins that render the normally transparent lens opaque. Such changes may occur in dogs or cats of any age for a variety of reasons (eg, congenital, traumatic, post-inflammatory, metabolic, nutritional, age-related) and by a variety of pathophysiologic mechanisms, with the end results being obstruction of the visual pathway and subsequent vision deficits.1
In addition, chronic intraocular inflammation, secondary glaucoma, and associated discomfort or pain may result from cataracts. The degree of vision impairment depends on the extent of the cataract. Incipient cataracts occupy <10% to 15% of the lens and are associated with minimal vision impairment. Immature cataracts that occupy from 15% to 95% of the lens and mature cataracts that occupy 100% of the lens are associated with more significant deficits.1 Hypermature cataracts involve leakage of lens proteins into the eye and can progress to apparent shrinking of the cataract (ie, morgagnian cataract) and may in turn be associated with improved vision. Hypermature and morgagnian cataracts are frequently associated with chronic lens-induced uveitis, thus coinciding damage to the globe may limit visual ability in those patients.
The Difference
Nuclear sclerosis is commonly confused with cataracts but is different in both the cause and effect on the patient. This age-related change is common in dogs (50% of dogs over approximately 9 years of age2) and cats, as continued formation of normal lens fibers compresses the central nucleus, leading to increased nuclear density. In contrast to cataract, nuclear sclerosis is not considered to cause vision deficits. However, it can cause a visible cloudiness to the lens that can be confused with cataracts.
Management Approaches
Accurate distinction of cataracts and nuclear sclerosis is necessary for appropriate management. Cataracts may cause lens-induced uveitis, necessitating chronic topical anti-inflammatory therapy and may be corrected by surgical removal. Cataracts may also be indicative of an underlying disorder that needs to be identified and addressed. Nuclear sclerosis causes neither vision deficits nor inflammation; therefore, treatment is not indicated and no further diagnostic testing is required.
Differentiation Tactics
Differentiating cataracts from nuclear sclerosis can be most easily achieved during the eye examination by either distant direct ophthalmoscopy or distant illumination. Distant direct ophthalmoscopy utilizes the tapetal reflection to retroilluminate (backlight) the lens and associated opacities; distant (or diffuse direct) illumination involves shining light directly on the surface of the lens.3 Both use the tapetum to retroilluminate the degree of obstruction of the visual axis.
Step-by-Step: Differentiating Between Cataracts & Nuclear Sclerosis
What You Will Need
Focal light source (direct ophthalmoscope or transilluminator; Figure 1)
Tropicamide 1% (short-acting mydriatic agent)


FIGURE 1 Direct ophthalmoscope (A) and transilluminator (B). Both serve to provide a focal light source that allows visualization of ocular structures.
Step 1
Perform visual inspection of the eye with a light source to determine overall ocular health and clarity.
Author Insight
Gross visual inspection of each eye is critical, as opacities in other structures of the eye, such as the cornea, anterior chamber, or vitreous, will also obscure the tapetal reflection and could be confused with cataracts.
Step 2
Ideally, evaluation of intraocular pressure (IOP) via applanation or rebound tonometry will occur prior to instillation of the mydriatic agent. If the IOP is elevated (>20 mm Hg), caution should be exercised and administration of the mydriatic agent should be avoided.
Step 3
If the IOP is normal, instill a single drop of tropicamide 1% in each eye; this should produce adequate dilation for thorough evaluation of the lens within 10 to 15 minutes.
Author Insight
Dilation of the pupil is important to enable visualization of the majority of the lens, which is important as cataracts at the lens equator (peripheral portions of the lens) are unlikely to be visualized in the absence of mydriasis.
Step 4
With the room lights dim, the light source is placed as close to the examiner’s visual axis as possible, and from arm’s length distance, the light is directed toward each of the patient’s eyes. If using a direct ophthalmoscope, the examiner looks through the ophthalmoscope (distant direct ophthalmoscopy), whereas if using a transilluminator for direct illumination, the transilluminator may be placed at the examiner’s temple (Figure 2).
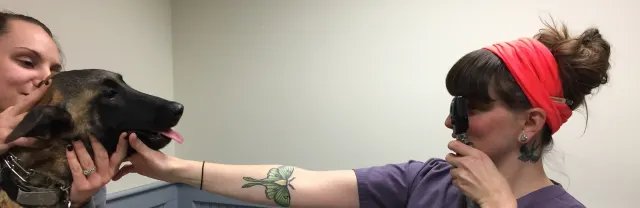
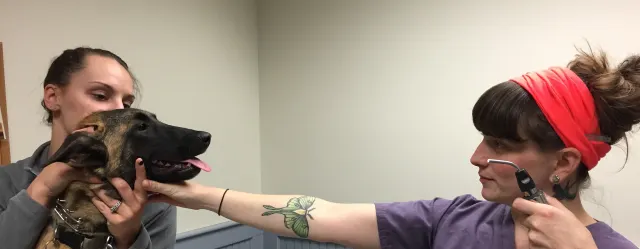
FIGURE 2 Placement of ophthalmoscope directly in front of the examiner’s eye for distant ophthalmoscopy (A) vs placement of transilluminator beside the examiner’s eye for diffuse, distant illumination (B). Both setups place the light in the path between the examiner’s and patient’s eyes and can be used to obtain visualization of the tapetal reflection (retroillumination). (Note: For the purposes of the image, the room lights were left on; however, the room should be darkened when performing these techniques.)
Author Insight
Keeping the light source dim improves comfort for the patient, thus also improving compliance with the examination. Darkening the room also improves contrast and reduces the reflection of room lights in the tear film, improving recognition of the tapetal reflection.
Step 5
Visualize the tapetal reflection to determine if obstruction of the visual axis is present.
Author Insight
Visualization of the tapetal reflection requires the examiner be directly in line with the patient’s visual axis, which may necessitate moving either the examiner or the patient in order to identify when the correct orientation is achieved.
Step 6
If obstruction is present and can be localized to the lens based on gross visual inspection of the eye, then the diagnosis is cataract and appropriate staging can occur (incipient, immature, mature, or hypermature; Figures 3 and 4).



FIGURE 3 Normal lens (A) and incipient (B), immature (C; patient’s right eye), and mature (C; patient’s left eye) cataracts, as identified by retroillumination and as would be seen utilizing distant direct ophthalmoscopy.
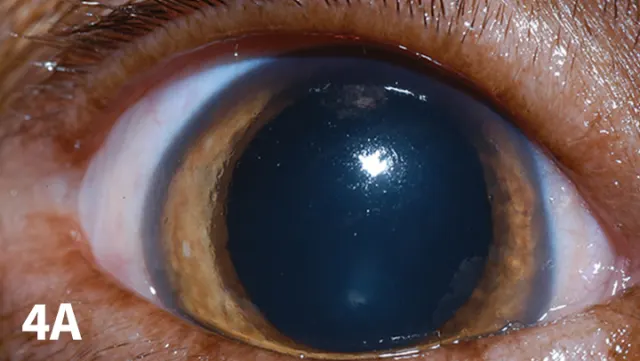
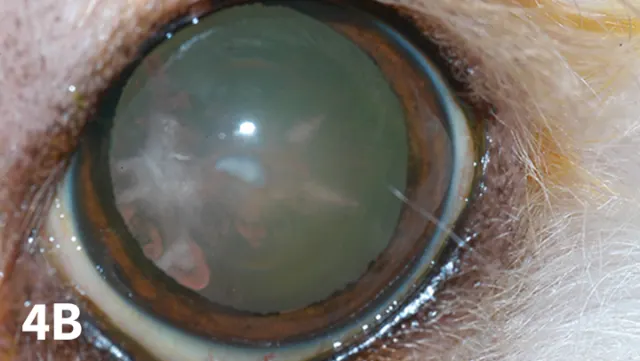

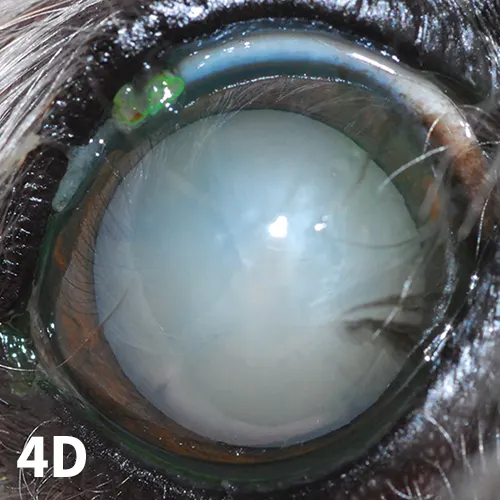
FIGURE 4 Clinical photographs demonstrating normal lens (A) and incipient (B), immature (C), and mature (D) cataracts, as identified by direct illumination.
Step 7
If obstruction is not present but central lens has cloudiness to it with a distinct nuclear or cortical junction (Figure 5), then the diagnosis is nuclear sclerosis.
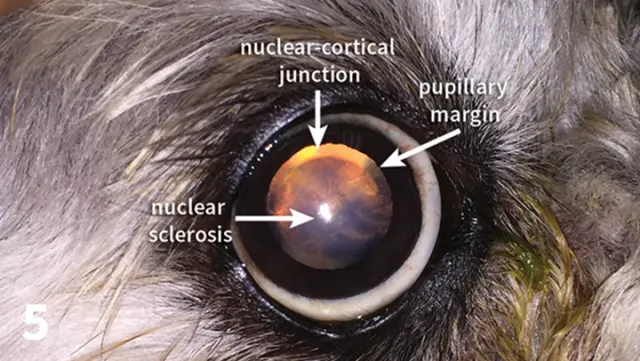
FIGURE 5 Clinical photograph demonstrating nuclear sclerosis via distant retroillumination. The junction between the lens nucleus and cortex is visible within the pupillary aperture, and the nucleus demonstrates a hazier appearance than the surrounding cortex, as seen by faint alteration of the tapetal reflection.