Chordae Tendineae Rupture in a Dog
Amara H. Estrada, DVM, DACVIM (Cardiology), University of Florida
Case Scenario
An 8-year-old spayed bichon frise presented for acute onset tachypnea and dyspnea discovered upon the client’s return from work. The patient was on regular flea, tick, and heartworm preventatives, but had not seen a veterinarian in 2 years.
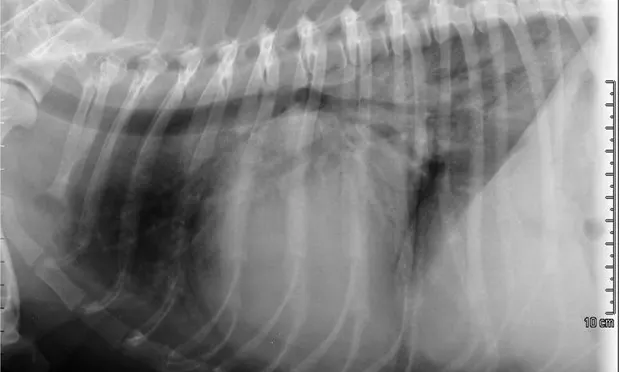
A murmur and regular rhythm were auscultated. The heart rate was approximately 180 bpm, and crackles were auscultated in the caudodorsal lung fields. A 6 lead electrocardiogram (ECG, Figure 1) and thoracic radiographs (Figure 2A and 2B) were performed.
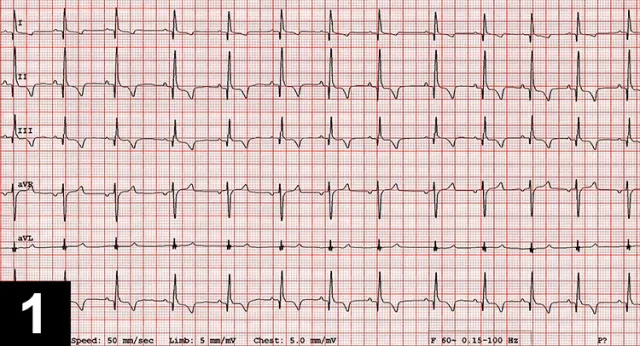
Figure 1 6 lead ECG
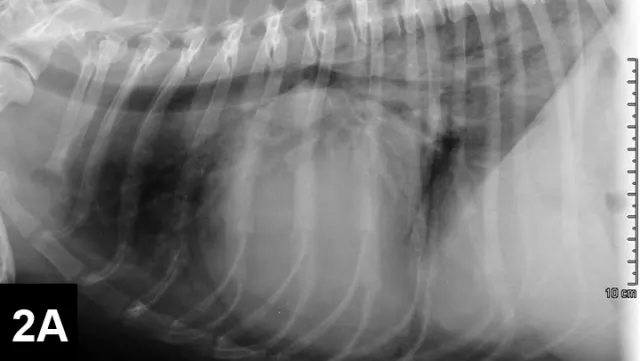
Figure 2A Right lateral thoracic radiograph

Figure 2B VD thoracic radiograph
Diagnostics
A sinus rhythm (HR is ~150 bpm) and left ventricular enlargement pattern were noted on ECG: the sensitivity was decreased to 5 mm/mV, and R waves measured ~3 mV (upper end of normal R-wave height is 2.5 mV). Thoracic radiographs revealed severe left atrial enlargement with moderate left ventricular enlargement. There was a moderate interstitial to alveolar pulmonary pattern most pronounced in the caudodorsal lung fields, which is consistent with left-sided congestive heart failure resulting from degenerative mitral valve disease.
Initial Diagnosis
Based on the signalment, physical examination, ECG, and thoracic radiographs, a presumptive diagnosis of degenerative mitral valve disease was made. The patient was placed in an oxygen cage; nitroglycerin paste (¼ inch strip) was applied to the inner ear, and intramuscular injections of furosemide (4 mg/kg) were administered every hour until the patient was no longer dyspneic and could lie down comfortably (total of 3 IM doses). An IV catheter was placed, and a small amount of blood from the catheter hub was used to run an in-house renal panel; BUN, creatinine, and electrolytes were all within normal limits. Administration of furosemide was continued at 3 mg/kg IV q4h through the evening (3 additional doses total), nitroglycerin (¼ inch strip) was applied topically to the ear q12h, and pimobendan 0.3 mg/kg was administered orally q12h. The following morning, the patient rested comfortably, but the respiratory rate remained >60 bpm. Repeat thoracic radiographs showed a reduction in the degree of pulmonary edema. Renal values were mostly unchanged. Systolic blood pressure was measured by Doppler at 160 mm Hg. At this point, the patient could tolerate short durations outside the oxygen cage.
A brief echocardiogram showed severe left atrial and left ventricular volume overload. The mitral valve was severely thickened and degenerative, and there was severe prolapse of the entire valve and an apparent flail segment (Video 1A and 1B) of the anterior mitral valve (ie, tips of the leaflet pointed into the left atrium during systole). With color Doppler, a wide jet of severe mitral insufficiency was identified (Video 2).
Based on cursory imaging, a diagnosis of severe degenerative mitral valve disease with probable acute chordae tendineae rupture or tear and development of acute heart failure was made. Because blood pressure was documented to be at the high end of the normal range despite therapy with pimobendan (a potent vasodilator and inotropic agent), further afterload reduction was achieved with IV nitroprusside administered via constant rate infusion (1–10 micrograms/kg/min uptitrated to achieve a systolic blood pressure between 110-130 mm Hg). Diuretic therapy was continued with 3 mg/kg of furosemide IV q6h. Pimobendan and nitroglycerin were continued as above. After another 24 hours, the patient was eupneic and able to exit the oxygen cage. The nitroprusside was gradually tapered and discontinued, and the patient was started on oral medications including 2 mg/kg furosemide PO q8h, 0.3 mg/kg pimobendan PO q12h, 2.5 mg amlodipine PO q12h, and enalapril 0.5 mg/kg PO q12h.
Chordae tendineae rupture resulting from degenerative mitral valve disease is classically described as a devastating complication of canine mitral valve disease responsible for acute left heart failure, which commonly results in pulmonary edema. It was previously associated with very poor short- and long-term prognoses. A retrospective study in the Journal of Veterinary Medicine in 20071, however, showed that dogs with chordae tendineae rupture had a mean survival time of 425 days from initial diagnosis, which was longer than previously thought and similar to that of dogs with heart failure resulting from mitral valve disease without chordae tendineae rupture. Although chordae tendineae rupture is severe, successful management is possible, and dogs may have a good quality of life following the initial heart failure. Key components of disease management include:
Aggressive therapy, including cage rest, supplemental oxygen, high dose IM or IV furosemide (4–6 mg/kg q1-4h initially), and oral pimobendan, if it can be safely administered orally. Gentle handling is crucial in these fragile patients.
A quick diagnosis or suspicion of the disease, which should be among the differential diagnoses for dogs with a long-standing murmur and acute development of heart failure. Although echocardiogram may not be readily available, blood pressure should always be measured if a patient with left-sided heart failure is not improving on aggressive diuretic therapy. If the systolic blood pressure is greater than 150 mm Hg, afterload reduction should be considered early to reduce the regurgitant volume, decrease left atrial pressure, and speed resolution of pulmonary edema. Nitroprusside (intravenous) is a potent arteriodilator that must be administered via constant rate infusion. Because nitroprusside has a very quick half-life, its effects can be quickly reversed by decreasing the dose if hypotension occurs. Hydralazine is another potent arteriodilator that can be administered orally and that has a relatively quick onset of action; however, if clinically important hypotension occurs, it may take several hours to reverse. Amlodipine is a vasodilator that can reduce the afterload and decrease the regurgitant fraction, but its onset of action is slower, making it less useful in emergency settings.
If an ultrasound unit is available, learning basic echocardiographic views can be very beneficial for making subjective assessments. The diagnosis of a torn or ruptured chordeae tendineae is not particularly difficult if the basic right-sided imaging planes are known and the practitioner is comfortable with the appearance of a normal mitral valve. Basic echocardiographic imaging can also assist in assessments of contractility, chamber size, and the presence or absence of pleural or pericardial fluid.