Abdominal Effusion in a Dog
Mandy Meindel, DVM, Kansas State University
Lisa M. Pohlman, DVM, MS, DACVP, Kansas State University

A 2-year-old, spayed toy poodle mix presented with a distended abdomen.
History
The dog had been seen by the referring veterinarian for a 2-month history of intermittent vomiting. Diagnostic testing (eg, CBC, serum biochemistry profile, radiography) was inconclusive; exploratory laparotomy revealed no significant findings. Biopsies were not performed. Progressive abdominal distention became apparent in the 2 weeks following surgery, and the patient was referred to local specialists.
Physical Examination
The dog was quiet, alert, and responsive. In addition to a distended abdomen, jaundice mucous membranes were present. Temperature (102.2°F) was normal, but heart and respiratory rates were increased at 220 bpm and 60 breaths per minute, respectively.
Diagnostics
CBC showed mild lymphopenia (0.9 103/µL; reference, 1.0–4.8 103/µL) and moderate thrombocytosis (654 103/µL; reference, 200–500 103/µL). Serum biochemistry profile revealed mildly increased ALP at 269 U/L (reference, 20–150 U/L), moderately increased ALT at 218 U/L (reference, 10–118 U/L) and total bilirubin of 2.3 mg/dL (reference, 0.1–0.6 mg/dL), and mildly decreased total protein of 4.6 g/dL (reference, 5.4–8.2 g/dL) and globulin of 1.9 g/dL (reference, 2.3–5.2 g/dL).
Radiography revealed diffuse fluid opacity in the abdomen. Abdominocentesis was performed (See table Abdominal Fluid Analysis). Figures 1–3 are low- and high-power, respectively, photomicrographs of cytocentrifuged (concentrated) preparations of peritoneal fluid.
Cytology
Cells (Figures 1–3) consisted of ~70% macrophages containing gold and dark brown to black pigment, ~30% mildly degenerate neutrophils, scattered erythrocytes, and rare squamous debris (likely contaminant). Gold amorphous material was observed in the background. No microorganisms were identified.
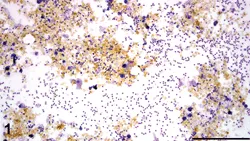
Gold amorphous pigment was present in the background with scattered inflammatory cells and erythrocytes. (Modified Wright stain; 200× original magnification)
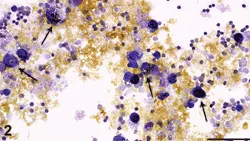
Macrophages frequently contain gold to black pigment (arrows). Gold amorphous pigment, scattered inflammatory cells, and erythrocytes were also present. (Modified Wright stain; 600× original magnification)
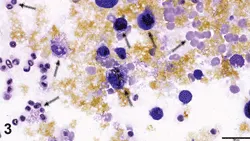
Macrophages (black arrows) contained gold pigment (consistent with bile) and dark brown to black pigment consistent with breakdown products of bile and/or hemosiderin (if mild concurrent hemorrhage occurred). A degenerate neutrophil (red arrow) and small lymphocytes as well as frequent erythrocytes (green arrows) were present. Gold amorphous pigment was also observed in the background. (Modified Wright stain; 1000× original magnification)
Ask Yourself
1. What type of effusion is present?2. What is the significance of the gold and dark brown to black pigment observed in Figures 1–3?
Diagnosis
Bile Peritonitis
Bile peritonitis is an inflammatory response to bile leakage into the peritoneal cavity.1 Bile leakage may occur spontaneously or as a result of:
Dehiscence of a biliary tract incision
Failure of cystic duct, bile duct, or hepatic duct ligatures
Rupture of the gallbladder or biliary tract secondary to calculi, cholecystitis, manipulation, neoplasia, pancreatitis, or trauma.2,3
Bile salts can cause chemical peritonitis, resulting in permeability changes and tissue necrosis.4 Initially, without a smear of the fluid, total nucleated cell count and total protein of peritoneal fluid can often suggest a protein-rich transudate (ie, modified transudate). However, presence of abundant gold pigment with macrophages and degenerate neutrophils on cytologic preparation is indicative of bile leakage with secondary inflammation. With time, the bile will incite a moderate inflammatory response typical of an exudative process (ie, high total nucleated cell count, high total protein).
Clinical signs of bile peritonitis typically include anorexia, vomiting, diarrhea, weight loss, icterus, abdominal distention, fever, and abdominal pain.2 Signs can often be more chronic with biliary rupture than with gallbladder rupture. Immediately after bile duct rupture, dogs often have minimal or no signs. Abdominal distention may slowly occur over 1 to 2 weeks.3
Treatment & Prognosis
Surgical repair is required to stop the flow of bile into the peritoneal cavity. Abdominal lavage to remove bile and reduce the inflammatory stimulus can speed recovery. Abdominal drainage may be needed to remove postoperative fluid accumulation. If secondary bacterial infection is present, anaerobic and aerobic bacterial culture and sensitivity testing of fluid may help determine therapeutic choices. With treatment, prognosis is excellent unless bacterial infection is present, in which case survival rates may be 27% to 45%.2
Outcome
In this case, the bile duct was lacerated, presumably from manipulation during exploratory laparotomy. The bile duct was surgically repaired and the dog recovered uneventfully.
Did You Answer?
1. Despite low nucleated cell count, the effusion was classified as bilious exudate because of the bile and types of cells present (eg, macrophages often containing bile, degenerate neutrophils).2. The gold amorphous pigment observed within the macrophages and extracellularly was most consistent with bile. The dark brown to black pigment was most consistent with breakdown products of bile and/or hemosiderin (if concurrent mild hemorrhage has occurred).
Abdominal Fluid Analysis & Bile Peritonitis

Diagnosis of bile peritonitis can often be based on abdominal fluid analysis. A yellow–green color can usually be observed grossly in the fluid. Depending on leakage severity and resultant peritonitis, the fluid may appear hazy or cloudy. The nucleated cell count and total protein may vary, depending on whether the effusion is acute or chronic; with time, more inflammatory cells and protein will leak into the fluid. It is essential to evaluate both direct and concentrated cytologic fluid preparations to ensure that bile peritonitis has not been missed.
Concentrated preparations of effusions can be easily analyzed by centrifuging the fluid and making a smear of the sediment. Air-dried smears should be stained with Romanowsky stain (ie, Diff-Quik) and viewed microscopically. Microscopically, the cellular infiltrate will typically consist of neutrophils and macrophages. The characteristic gold, yellow, tan, blue–green, or dark brown to black pigment or bilirubin crystals may be observed in the background or intracellularly within macrophages. Once bile peritonitis is suspected, the total bilirubin concentration of collected fluid should be determined via an in-house chemistry analyzer or by submitting the fluid in a red-top tube (without serum-separator gel) to a reference laboratory. If the concentration is greater than that of the serum, bile peritonitis can be confirmed. In healthy animals, no bilirubin will be found in the abdominal fluid.4